One night in the ER
Like all medical professionals, staff members at Pullman Regional Hospital are doing their best to keep up with an increasingly hectic workload
PULLMAN — When the emergency department at Pullman Regional Hospital starts getting full, patients are put in “rooms” in the hallway — that is to say, gurney beds with their “room number” taped to the wall.
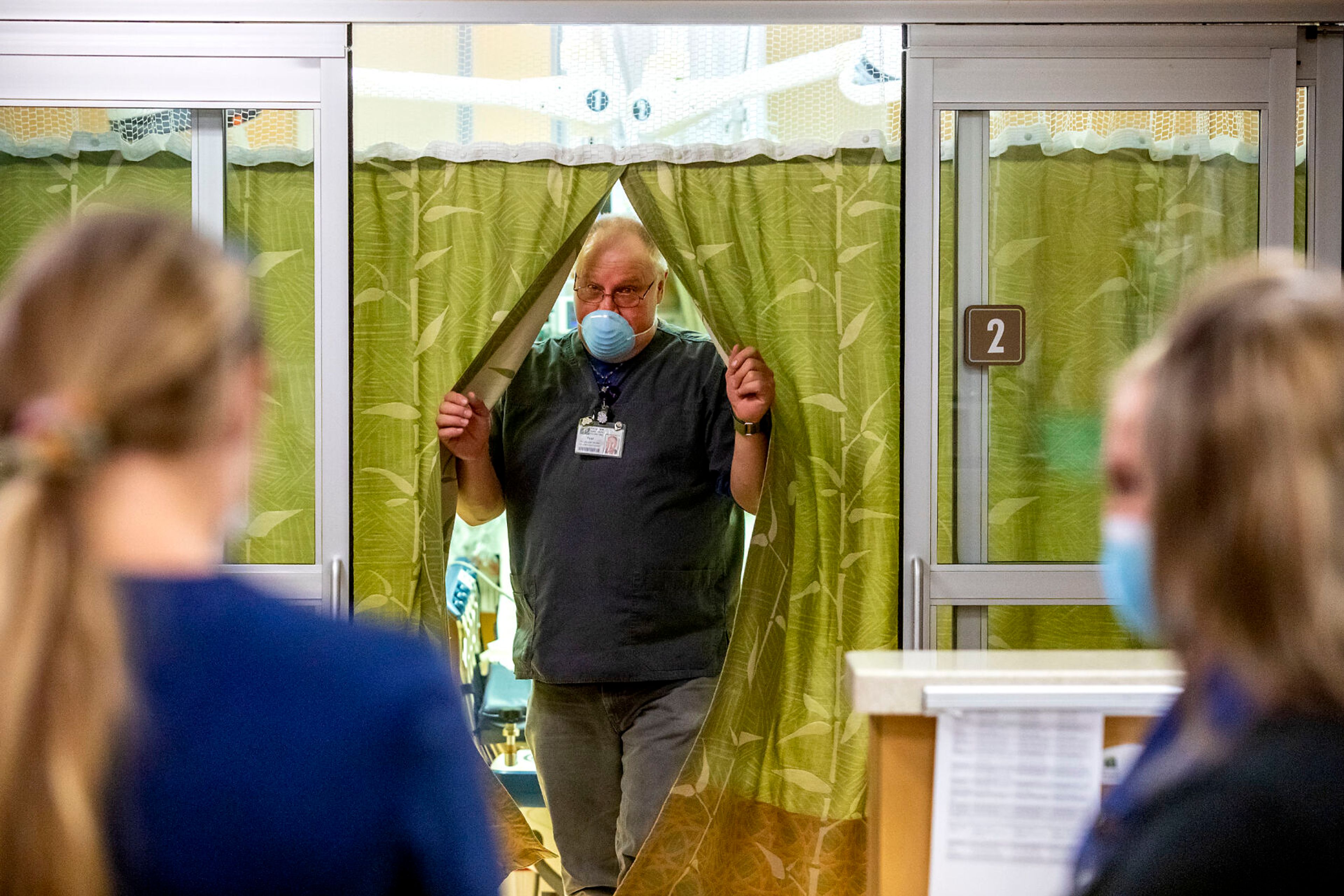
ER nurse Kelsey Erwin is walking through the hall on a Saturday night earlier this fall, pointing to different rooms and describing their function. Including the gurneys, there’s about 13.
When Erwin started at the hospital almost 10 years ago, the department rarely got busy, she said. But now, staff are often stuck working in tight quarters while trying to treat their patients.
“At night, we don’t often fill up every room, but it looks like clearly in the daytime, they’re literally putting three people to a hall,” she said. “Which is pretty stuffed.”
In severe cases, such as shootings, the lack of space can directly affect other patients’ experience, Erwin said. She’s treated gunshot victims twice since September of last year.
On one of those occasions, staff had to move patients to the hall gurneys to make room. One patient that night decided to discharge and come back the next day, and another who’d come in for stomach pain had to be moved to a spot where she could hear the patient with the gunshot wound being treated, and later pronounced dead.
“She probably still thinks (about that),” Erwin said. “I still think about that, and I’ve been doing this for 10 years. So for her to kind of have a front-row seat to something so tragic — it was hard.”
That same night, a psychiatric patient had to leave because the sounds were too overwhelming.
“We couldn’t stop him,” Erwin said. “So we had to just let him go and hope that he would come back.”
Luckily, not every night is so chaotic. On this particular Saturday, despite it being hours after a Washington State University home football game, the ER was unusually quiet, with one patient who dislocated his shoulder, and another, affectionately dubbed the “dancing king,” being treated for a wrist injury he sustained while breakdancing during a tailgate gathering in a parking lot. Another patient accidentally cut his arm smashing a TV after the Cougars lost their game.
Erwin said the mornings after game days, when patients who came in drunk wake up, can be one of her favorite times to work.
“They’re actually very sweet. It’s my favorite time of day. It’s kind of when you see, like, who they actually are versus the drunk, belligerent fool they were the night before. They’re usually very apologetic, Snapchatting pictures of their diapers to their friends.”
But even though they don’t always need extra rooms, Erwin said when they do, it’s hard to make up for the lack of workable space.
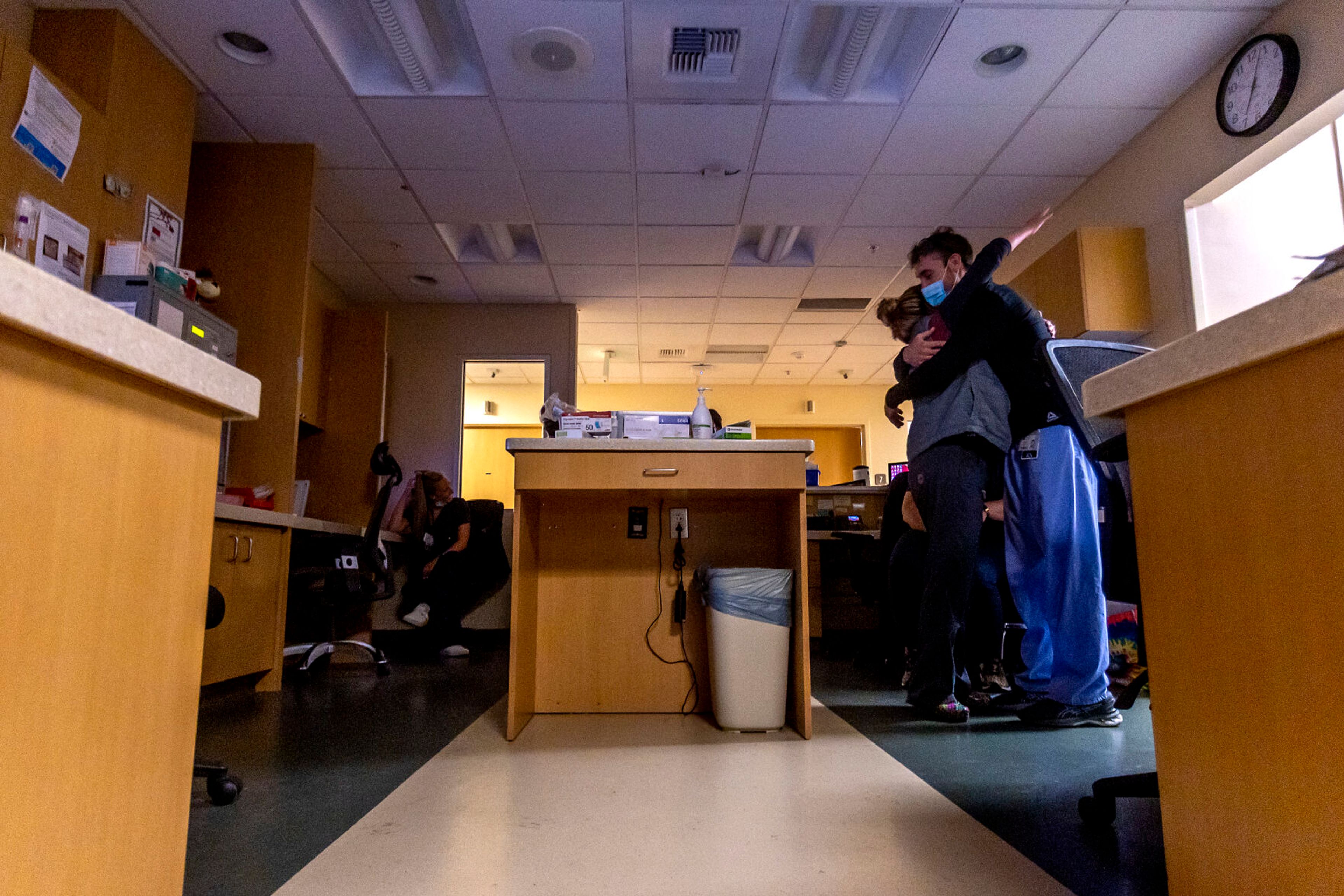
Sometimes, she said, staff have been forced to “run code” (a term describing immediate, life-saving care for patients in cardiac arrest) in small exam rooms.
“If there’s six to 10 people trying to save a life, these rooms get pretty tight,” she said. “So that’s a concern that we have, too.”
It’s a problem that’s been growing for years. Paul Prather, another ER nurse, said he’s seen the number of patients more than double since he started in 2013.
“We’re seeing older, sicker clientele, we’re seeing more psych patients with debilitating psych issues that are taking up a lot of our time,” Prather said. “It used to be that you’d see 40 or 45 patients in a 24-hour time span. And it’d be like, ‘Wow, that’s a busy day.’ And now we’re seeing 40 to 70, just on day shift.”
In August, the ER had its fourth straight month of record volume, treating 1,276 patients.
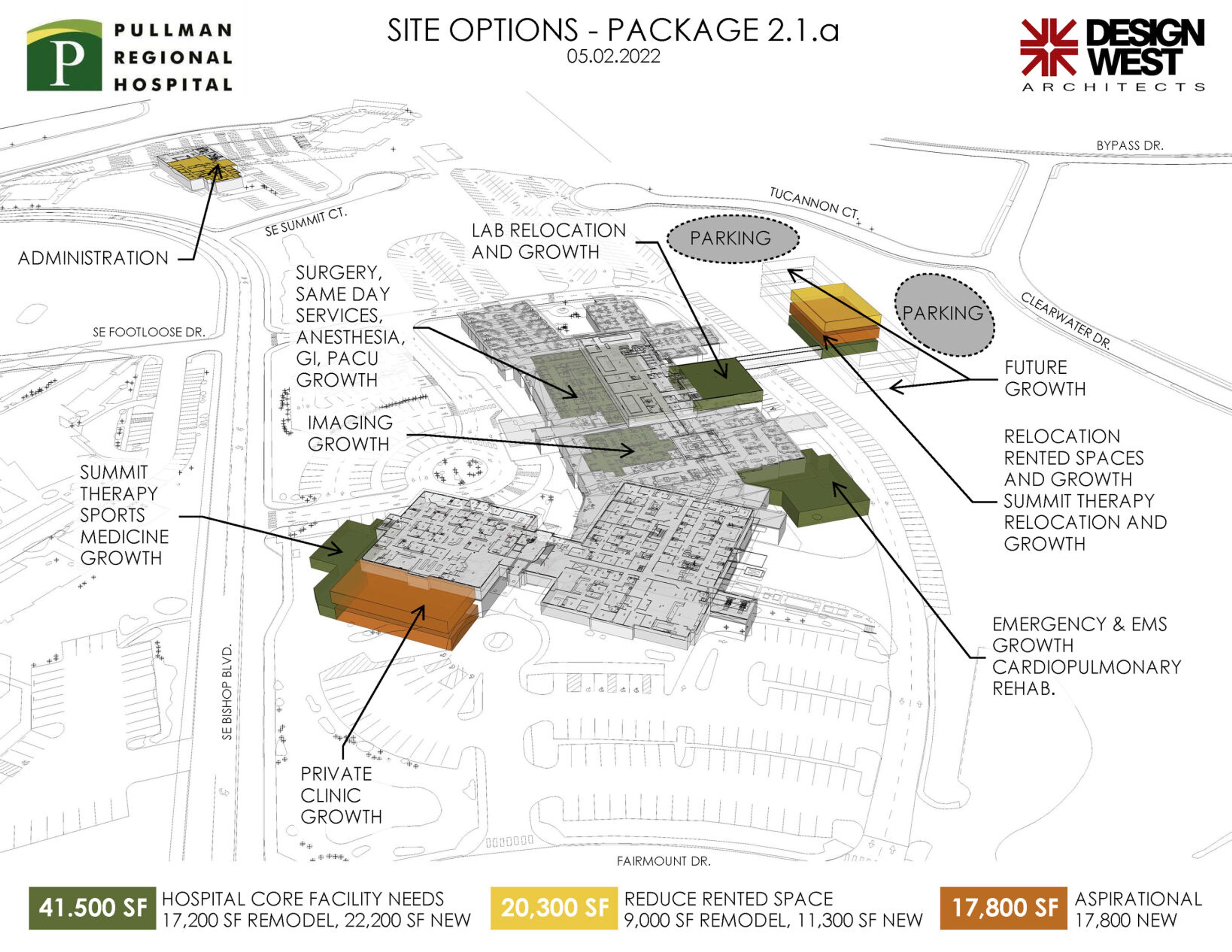
Hospital staff are hoping a $27.5 million bond this November will help them get more space and resources to do their job. The hospital’s expansion plan is vast, but one of the biggest line items is a 50%-60% expansion of the ER for triage rooms and mental health services.
Resources for psychiatric patients have been one of the fastest-growing needs over the past decade, staff said.
They’ve seen even more over the pandemic, Erwin said. Many are students who were socially isolated the last three years.
“Then their parents are sending them away to college, and it’s going very poorly for them. So we see a lot of psychiatric emergencies. And this,” Erwin said, pointing to a small, closed-in room, “is where we have to put them. And it’s just — it doesn’t help anyone to be locked in this little room, you know? So we would love to be able to provide them with better care, especially just the influx of them that we’re seeing.”
The ER has one psychiatric room, which is also the only room with video monitoring and restraint capabilities, though the restraints aren’t typically used. When additional psychiatric patients need a room and the first is occupied — which often happens — they’re set up in two other rooms within eyesight of the nurses’ station.
“Oftentimes all of those rooms are full, and the capacity for psychiatric beds in the state is pretty low,” Erwin said. “So we’re often holding them for 12, 24 hours if they need a real psychiatric bed.”
The hospital ER also frequently ends up treating patients that need to be transferred to an intensive care unit bed, Erwin said. But the availability for those beds are often few and far between.
“We’re not ICU nurses,” Erwin said, “but we sure turn into them pretty quickly when we have to.”
Sometimes, it can take 12 to 24 hours before they find an available bed to transfer a patient, Prather said.
“One we were trying to transfer the other day (where) we talked to Seattle, Spokane, Missoula, Boise, I don’t know where else — Lewiston — you just — nobody’s got open ICU beds,” he said.
One of the most challenging times in the ER is when a victim of sexual assault comes in for evidence collection, Erwin said.
Fall is usually the worst time for those patients, with game days and frequent parties likely contributing to more cases. Erwin said she knew of two cases where a patient had come in for evidence collection in the last week alone.
Those cases take time, and ER staff aren’t just dealing with assault survivors from the Pullman area. Often, patients are sent from the Lewiston-Clarkston Valley when their own hospitals don’t have a nurse available for the job, she said.
“We try to do our best to do a thorough exam to help collect evidence. And that takes about four hours,” she said. “It really can get dicey when we’re busy. And we need an entire room. And we need somewhere that’s quiet, to be able to provide the kind of care that they need at that time.”
Erwin said she can’t imagine her life without nursing, and loves her job. But more resources would make it easier to provide necessary treatment.
If staff need to run code and fit 10 people in an exam room, they’ll make it happen, she said. But it’s not ideal for her, and it’s not ideal for her patients.
“We can do it,” she said. “But we don’t like it.”
Sun may be contacted at rsun@lmtribune.com or on Twitter at @Rachel_M_Sun. This report is made possible by the Lewis-Clark Valley Healthcare Foundation in partnership with Northwest Public Broadcasting, the Lewiston Tribune and the Moscow-Pullman Daily News.